Prenatal visits have been recognized as a window of opportunity to deliver healthcare and prevention to reduce obstetric complications and adverse birth outcomes, which is particularly important for the subpopulations characterized by socially disadvantaged backgrounds and high-risk conditions (e.g., women involved in illegal drugs). With the rising number of women with opioid use disorders (OUD) worldwide, Dr. Chuan-Yu Chen, a Join Appointed Investigator with the Center for Neuropsychiatric Research, investigated the inappropriate utilization of prenatal services among women attending the methadone treatment and explored sociodemographic and clinical characteristics associated with prenatal visits and early entry into prenatal services in Taiwan.
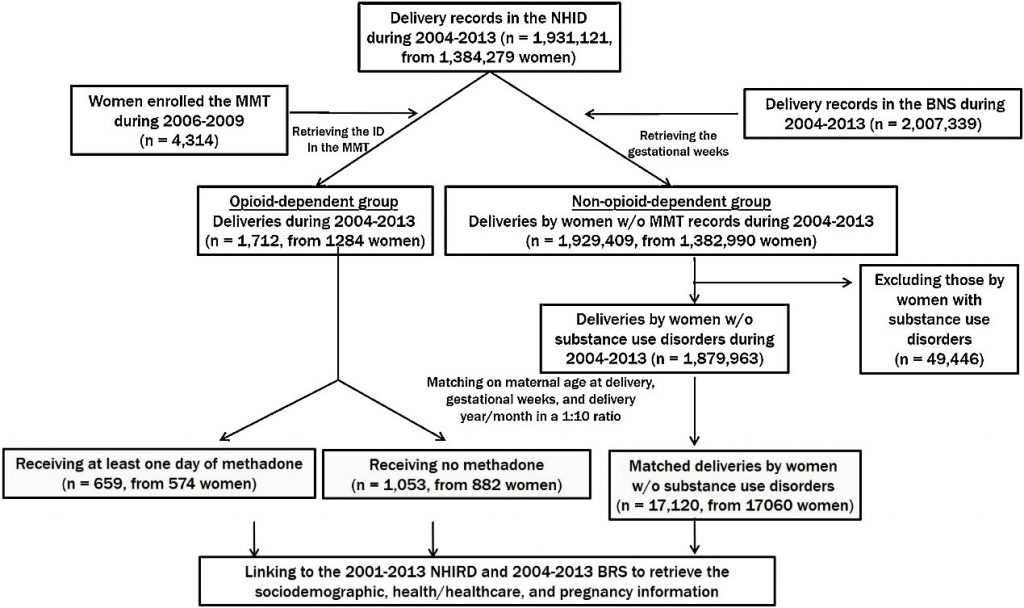
A total of 1712 pregnancies with 20 or more gestational weeks from women enrolled in the methadone maintenance treatment (heroin-exposed: receiving no methadone treatment during pregnancy, n = 1053 by 882 women; methadone-treated: receiving methadone for at least one day during pregnancy, n = 659 by 574 women and their 1:10 matched pregnancies from 17,060 women without substance use disorder in the period of 2004-2013) have been identified from 4 national administrative databases (the Methadone Maintenance Treatment (MMT) register with national health insurance, national birth notification system, and birth registration system) .The generalized linear mixed models with negative binomial and logit distributions were conducted to evaluate the relationship between individual sociodemographic, health, and addiction treatment characteristics with the number of prenatal visits and receiving prenatal care in the first trimester (i.e., early entry).
The analyses found 80% of pregnancies by women with OUD received no prenatal services and 21% had started prenatal care in the first trimester as compared with 1% and 46% in pregnancies by women without substance use disorders. For pregnancies by women with OUD, methadone treatment was not linked associated with prenatal care visits (adjusted relative risk [aRR] = 1.02; 95% = 0.92, 1.12). For methadone-treated pregnancies, treatment enrollment before pregnancy and spousal methadone treatment elevated prenatal visits by 8% and 18% (0.48 and 1.08 visits, respectively). Additionally, HIV infection (adjusted odds ratio [aOR] = 0.30, 95% CI = 0.10, 0.83) and prior delivery (aOR = 0.05, 95% CI = 0.01, 0.19) significantly reduced the odds of early entry into prenatal care. These findings indicated an urgent need to integrate addiction treatment programs with prenatal care to increase adequate prenatal care for pregnant women with OUD, especially the HIV-affected or multiparous ones.
Citation: Chen, CY; Wang, IA; Fang, SY; Huang, N; Tsay, JH; Chang, SH. Inadequate prenatal care utilization among women with and without methadone-treated opioid use disorders in Taiwan. International Journal of Drug Policy. 2019 May;67:1-8.
